Maintaining healthy veins is crucial for overall vascular health and well-being. While genetics and other factors can influence vein health, adopting a balanced diet and regular exercise routine can significantly contribute to the prevention of vein issues such as varicose veins and chronic venous insufficiency. In this blog post, we’ll explore the vital role of diet and exercise in promoting healthy veins and provide practical tips to incorporate into your lifestyle.

The Importance of a Balanced Diet
A nutrient-rich diet supports overall vascular health by providing the essential vitamins and minerals needed for strong and flexible blood vessels. Here are some key dietary components that can benefit your vein health:
1. High-Fiber Foods
Dietary fiber helps prevent constipation, which can increase pressure on veins in the lower body and contribute to the development of varicose veins and hemorrhoids. Include plenty of fruits, vegetables, whole grains, and legumes in your diet.
2. Antioxidant-Rich Foods
Antioxidants help protect blood vessels from damage caused by free radicals. Foods rich in antioxidants, such as berries, citrus fruits, leafy greens, and nuts, can support vein health.
3. Omega-3 Fatty Acids
Omega-3 fatty acids have anti-inflammatory properties and can improve blood flow. Incorporate sources of omega-3s like fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, and walnuts into your meals.
4. Hydration
Staying well-hydrated is essential for maintaining healthy blood viscosity and preventing blood clots. Aim to drink plenty of water throughout the day.
5. Low-Sodium Diet
Excessive salt intake can lead to water retention and increased pressure on veins. Reduce your sodium intake by avoiding processed foods and using herbs and spices for flavoring instead.
The Role of Exercise in Vein Health
Regular physical activity is vital for promoting healthy blood circulation and preventing vein-related issues. Here are some ways exercise can benefit your vein health:
1. Improved Circulation
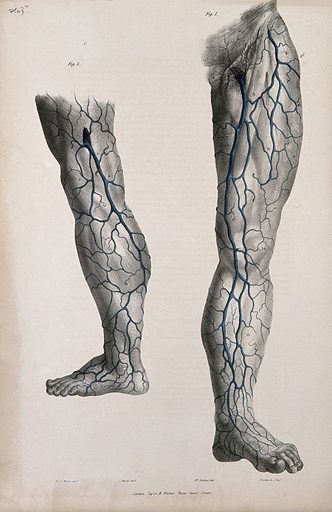
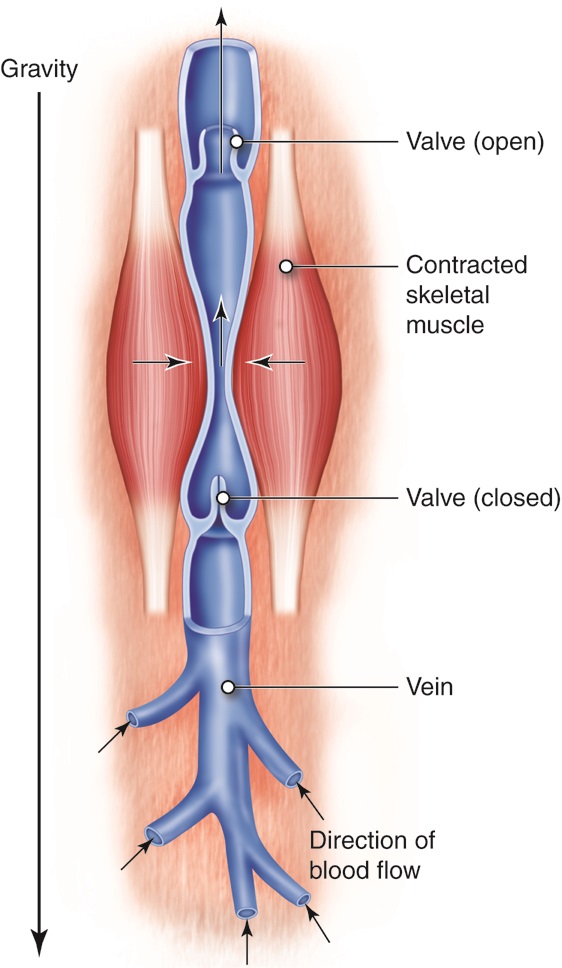
Exercise helps improve blood flow by strengthening the muscles that support your veins, particularly in the legs. Activities like walking, cycling, swimming, and jogging can enhance circulation.
2. Weight Management
Maintaining a healthy weight reduces the pressure on your veins and lowers the risk of developing varicose veins and other venous conditions. Regular exercise can help you achieve and maintain a healthy weight.
3. Reduced Venous Pressure
Physical activity prevents blood from pooling in the lower extremities, reducing the pressure on veins. This can help prevent the development of varicose veins and alleviate symptoms of venous insufficiency.
4. Strengthened Leg Muscles
Exercises that target the leg muscles, such as calf raises, squats, and lunges, can strengthen the muscles that help pump blood back to the heart, supporting healthy vein function.
Practical Tips for a Healthy Lifestyle
Incorporating diet and exercise into your daily routine can be straightforward with these practical tips:
1. Create a Balanced Meal Plan
Plan your meals to include a variety of nutrient-rich foods that support vein health. Focus on incorporating high-fiber foods, antioxidants, and omega-3 fatty acids into your diet.
2. Stay Active Throughout the Day
Find ways to stay active, even if you have a sedentary job. Take short breaks to walk around, stretch, and perform leg exercises. Aim for at least 150 minutes of moderate-intensity exercise each week.
3. Stay Hydrated
Carry a water bottle with you and set reminders to drink water throughout the day. Hydration is key to maintaining healthy blood flow and preventing dehydration-related vein issues.
4. Limit Processed Foods
Reduce your intake of processed and high-sodium foods. Opt for fresh, whole foods whenever possible and use herbs and spices to add flavor to your meals without excess salt.
5. Monitor Your Weight
Keep track of your weight and aim to maintain a healthy weight through a combination of diet and exercise. Consult with a healthcare provider if you need guidance on achieving your weight goals.
Contact Dr. Norman Chideckel for Maintaining Healthy Veins
For personalized advice on maintaining healthy veins through diet and exercise, consult with Dr. Norman Chideckel at the Vascular Surgery & Vein Center in New York City.
Dr. Chideckel can provide expert recommendations tailored to your individual needs, helping you achieve optimal vein health. To learn more and schedule a consultation, reach out to us at:
Dr. Norman Chideckel
Vascular Surgery & Vein Center of NYC
212-993-6133




 EVLT is an excellent treatment option for many individuals with varicose veins, but it may not be suitable for everyone. Factors such as the size and location of the veins, your overall health, and any underlying medical conditions will be considered by your vascular specialist to determine if EVLT is the best treatment option for you.
EVLT is an excellent treatment option for many individuals with varicose veins, but it may not be suitable for everyone. Factors such as the size and location of the veins, your overall health, and any underlying medical conditions will be considered by your vascular specialist to determine if EVLT is the best treatment option for you.
 In this blog we’ll explore effective tips and strategies to help you prevent varicose veins and maintain healthy veins. Varicose veins are swollen, twisted veins that often appear on the legs and can cause discomfort and cosmetic concerns. While genetic factors can play a role in the development of varicose veins, there are several lifestyle changes and preventive measures you can take to reduce your risk.
In this blog we’ll explore effective tips and strategies to help you prevent varicose veins and maintain healthy veins. Varicose veins are swollen, twisted veins that often appear on the legs and can cause discomfort and cosmetic concerns. While genetic factors can play a role in the development of varicose veins, there are several lifestyle changes and preventive measures you can take to reduce your risk.
 In this blog post, we’ll discuss the signs that you should see a vascular surgeon and when to seek help. Maintaining vascular health is essential for overall well-being, as the vascular system is responsible for transporting blood, oxygen, and nutrients throughout the body. However, certain symptoms and conditions may indicate underlying vascular issues that require professional evaluation and treatment.
In this blog post, we’ll discuss the signs that you should see a vascular surgeon and when to seek help. Maintaining vascular health is essential for overall well-being, as the vascular system is responsible for transporting blood, oxygen, and nutrients throughout the body. However, certain symptoms and conditions may indicate underlying vascular issues that require professional evaluation and treatment.


 What does post-surgery care for vein procedures look like? Undergoing vein procedures, such as sclerotherapy, endovenous laser treatment (
What does post-surgery care for vein procedures look like? Undergoing vein procedures, such as sclerotherapy, endovenous laser treatment (
