Do You Need A Varicose Vein Surgeon? If you have a job that requires you to stand for extended periods, you may develop varicosities or varicose veins. Many people are not aware of what varicose veins are, what causes it, and how you can identify if you have this condition. Well, note that vascular surgeons can treat this condition using surgical and non-surgical procedures.

(Source)
What Are Varicose Veins?
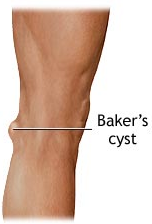
Varicose veins are a set of misshaped veins that become dilated due to excessive pressure, usually in the leg area. These veins are larger than usual veins and mostly appear as bluish-purple. Varicose veins are faulty veins that affect the blood flowing in the affected area. Thus, the veins become enlarge and get twisted into each other.
What Causes Varicose Veins?
Varicose veins may develop due to several reasons. Our body has a complex network of veins. The arteries circulate blood from your heart to the tissues. Next, the veins in the body pump the blood back to the heart for recirculation. Your vein legs play an essential role in the process and act against gravity.
However, when the leg veins don’t perform their task properly, you develop varicose veins. Damaged vein valves affect the blood circulation, and it begins to accumulate in the veins, making them enlarged. The most common reason is the excessive pressure on the lower body veins. Pregnant women and obese people are more prone to develop varicose veins.
What Are The Symptoms?
If you want to identify whether you have this condition, be aware of any signs of pain, irritation, the feeling of fullness, discoloration of the skin, and stiffness in one particular area. Besides, you may experience muscle cramps and swelling in legs and ankles.
These are a few of the symptoms of varicose veins that can also lead to spider veins. It is best to contact your doctor for examination and treatment if you observe any of these symptoms.
How Does A Varicose Vein Surgeon Treat This Condition?
There are many ways of treating varicose veins; however, the treatment would depend on the patient’s skin characteristics and whether they have any other health conditions. Maintaining a healthy lifestyle is one way of preventing varicose veins.
In worse cases, the surgeon may recommend undergoing surgical intervention. The four best ways to treat varicose veins in patients are:
Endovenous Laser Ablation
During this procedure, a specially trained surgeon will first numb the area and penetrate the vein using a catheter. The surgeon uses ultrasound for mapping the vein; he moves the catheter around the vein to the walls of the vein and seals it with thermal energy. Hence, the vein shuts, resulting in instant relief in some cases.
Once the EVLT is complete, the doctor will provide the patient with a compression stocking to place over the leg. It will allow circulation to improve. The benefit of this treatment is that it does not involve incisions. Hence, no stitches needed, and you can go about your day as normal.
Sclerotherapy
This procedure involves injecting a liquid into the vein. This results in irritating the wall of the vein; hence, causing the veins to collapse. The first step of the procedure involves cleaning the area where the injection will enter. Once the vein receives the injection, the patient might feel a burning sensation, or in some cases, nothing.
Surgeons don’t always use anesthesia during sclerotherapy and might even advise patients not to apply any lotion before the procedure.
Once the procedure is complete, the surgeon will gently massage that area to ensure the blood does not enter into that particular vein again. The doctor will also provide compression stocking to assist in proper blood flow.
This treatment does require a follow up to ensure there aren’t any more varicose or spider veins. A patient needs to avoid after this treatment is sunlight because that can cause dark spots on the treated area.
Phlebectomy
This procedure involves a small scalpel or needle, which will help make an incision in the skin where the vein is. The first step during this procedure is to numb the area with local anesthesia. The scalpel or needle will help penetrate the skin, making a tiny hole. After this, the surgeon will use a Phlebectomy hook to pull the vein out gently.
Once the procedure is complete, the surgeon will close the incision scar with a bandage. Therefore, the stitches won’t be needed.
Venous Ultrasound
This is another procedure surgeons opt for to understand the condition of the veins better. The ultrasound uses sound waves to detect how far the vein is and produce pictures of the veins. This ultrasound assists in searching for blood clots that might reside in the legs veins.
This procedure can help to understand the condition of the varicose veins and treat them with efficiency and safety.
Contact the Top Varicose Vein Surgeon in NYC Today
Remember, it is important that you discuss the best treatment for you with your doctor. If you’re looking for the best vascular surgeons to treat varicose veins, contact Dr. Norman Chideckel at the Vascular Surgery and Vein Center. We provide our patients with the highest level of care. Book an appointment to discuss your options and concerns about the treatments mentioned above.
Vascular Surgery & Vein Center
108 East 96th Street
Front 1
New York, NY 10128
212-993-6133