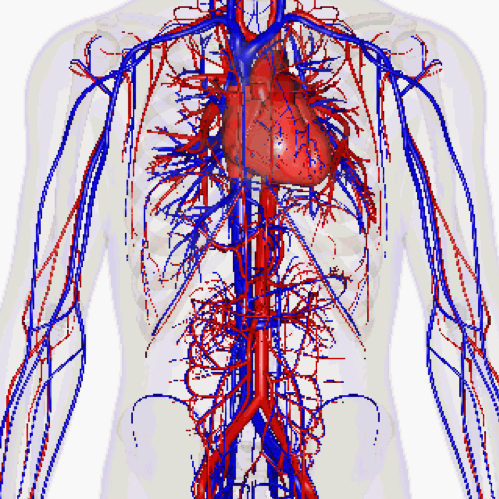
Arteries and veins are tube-like muscles that circulate blood throughout the body. Since blood pumping from the legs to the heart doesn’t receive any force, it uses valves. The valves prevent blood from moving backward.

The body’s arterial system is complex and causes numerous health problems. Below, we will discuss some health conditions related to arteries and veins:
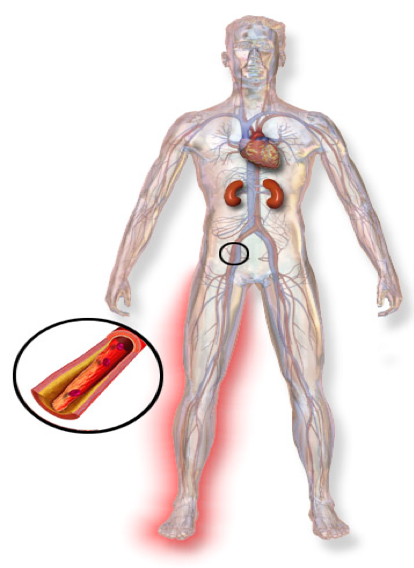
Deep Vein Thrombosis
Deep vein thrombosis is a condition caused due to blood clotting in the deep vein. Usually, the condition occurs in the leg because of weak blood flow. A study suggests that more than 900,000 people in the United States develop venous thromboembolism every year. Among those, up to 100,000 cases are fatal.
Surgery, hospitalization, cancer, and prolonged immobility can result in a blood clot. Also, if your family has a history of blood clotting disorder, you can develop this life-threatening condition. You can reduce the risk of DVT by consistently moving your body. For instance, exercise every day in the morning and avoid long sittings.
Atherosclerosis
Atherosclerosis and the hardening of the arteries prevent oxygen-rich blood from flowing throughout the body. You might develop this condition when plaque such as calcium, fat, or cholesterol builds up in the arteries. This condition disrupts the blood flow and causes serious conditions such as stroke or heart attack. If you have high cholesterol disease, you are at major risk for atherosclerosis.
You can prevent this condition by lowering heart disease risk factors. For instance, you can follow a healthy diet by consuming vegetables, fruits, and whole grains. Also, maintain a healthy weight. Reducing stress and avoiding cigarettes can also help.
Varicose Veins
A varicose vein and spider vein is a cosmetic condition that leads to severe disorder as well. These purple and swollen veins are common in women during pregnancy. Furthermore, both men and women over age 40 may develop the condition. Surveys suggest that more than 20 to 25 million people develop this condition in the United States.
Veins contain valves that maintain the blood flow and direct the blood in the right direction. However, if the valves fail to function for some reason, the blood will pool between two veins. Normally, varicose veins are not threatening. But, if you experience pain, burning, swelling, or itching, you need medical attention.
You can prevent varicose veins through physical activity. Also, you should maintain your weight and blood pressure to reduce the risk of varicose veins. Calf-strengthening exercises will help prevent varicose veins.
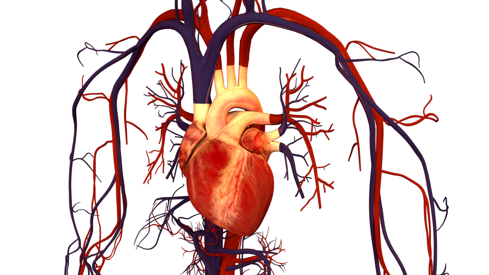
Coronary Artery Disease
Coronary artery disease or coronary heart disease is a common heart disease type. Every year, the condition takes about 370,000 people’s lives in the United States. CAD occurs when plaque accumulates in the arteries preventing oxygen-rich blood to reach the heart. This causes heart attack, chest pain, heart failure, or an irregular heartbeat.
High blood pressure, especially low HDL cholesterol, high cholesterol, or diabetes can cause CAD. You can choose a heart-healthy diet to reduce the risk of coronary artery disease. The heart-disease diet includes low sodium and saturated fat. Furthermore, regular exercising can also help. You should visit a professional vein specialist for complete diagnosis and treatment. They will prescribe medication to control high cholesterol and maintain blood pressure.

Peripheral Artery Disease
Peripheral arterial disease or PAD is a condition related to atherosclerosis. As the patient grows, the condition becomes worse. According to CDC, the condition affects more than 8.5 million people in the United States.
In this condition, the arteries that take blood from the heart to the legs narrow down because of plaque buildup. When the muscles receive low blood flow, it results in fatigue and pain in the legs. You might experience this problem while exercising or climbing stairs. Doctors can diagnose the condition through imaging tests. Furthermore, they compare blood pressure levels in the legs and arms.
High blood pressure, atherosclerosis, high cholesterol, and diabetes generate triggers the condition. Also, excessive smoking can lead to PAD. You can prevent this condition by exercising. Furthermore, maintain your cholesterol levels and blood pressure.
Arteries & Veins: Conclusion
If you experience symptoms of conditions related to veins, you can contact a professional vein specialist. Vein specialists diagnose your venous condition and recommend the best treatment plan. If you live in New York and want to consult experienced vein specialists, you can contact Vascular Surgery and Vein Center.
At the Vascular Surgery and Vein Center, our highly qualified surgeon Dr. Norman Chideckel will provide the most effective treatment for your venous condition. If you are in need of a consultation with our vein specialist, give us a call at .
Vascular Surgery & Vein Center
108 East 96th Street
Front 1
New York, NY 10128
212-993-6133